Table of Contents
- Introduction
- Core Pathophysiology: The Four Classical Pillars and Beyond
- 1. Sebum Overproduction and Sebaceous Gland Dynamics
- 2. Follicular Hyperkeratinization and Ductal Plugging
- 3. Microbial Colonization and Dysbiosis
- 4. Inflammation and Immune Response
- 5. Genetic and Epigenetic Predisposition
- 6. Metabolic, Dietary, and Hormonal Modulators
- 7. Environmental and Lifestyle Contributors
- 8. Psychological, Neuroendocrine and Psychosocial Interactions
- Integrative Etiologic Model (Synthesis)
- Research Updates and Gaps (Global and India-Relevance)
- Comments / Perspective from Renowned Dermatologists
- The Psychological and Chemical Interplay – More Depth
- Treatment Implications (Therapeutic Principles)
- Conclusion & Suggestions for Future Research
- References
- Our Other articles
Introduction
Acne vulgaris is among the most common dermatologic disorders worldwide, especially afflicting adolescents and young adults. Though much is known about its mechanisms, its etiology remains multifactorial and incompletely resolved. Understanding the precise causes is crucial—especially for integrating Ayurvedic insight with modern dermatology. In this article I examine in depth the current evidence on causation: genetics, endocrinology, microbiome, inflammation, environmental and psychological factors, and chemical changes in skin, with commentary on Indian studies and gaps. I conclude with a short note on how etiologic knowledge should guide therapy, though the focus remains on causation.

Core Pathophysiology: The Four Classical Pillars and Beyond
Modern dermatology commonly frames acne pathogenesis as an interplay of four primary processes (often called the “acne tetra”):
- Excess sebum production / sebaceous gland hyperactivity
- Follicular hyperkeratinization (impaired desquamation / plugging of the pilosebaceous duct)
- Microbial colonization (Cutibacterium acnes, formerly Propionibacterium acnes)
- Inflammation / immune response
However, more recent research has expanded this model to include genetic predisposition, hormonal / endocrine modulation, oxidative stress, barrier dysfunction, metabolic influences (insulin / IGF-1), environmental triggers, psychosocial stress and more. (PMC)
Below I dissect each component and then integrate newer research and Indian evidence.
1. Sebum Overproduction and Sebaceous Gland Dynamics
Sebaceous glands, found in association with hair follicles (pilosebaceous units), produce sebum—a lipid-rich mixture of triglycerides, wax esters, squalene, free fatty acids, cholesterol, etc. In acne, there is increased sebum output, which contributes to follicular blockage, creates a lipid milieu favorable for microbial growth, and interacts with inflammatory cascades.
Key drivers of increased sebum:
- Androgens: Testosterone, dihydrotestosterone (DHT), and other androgenic hormones stimulate sebaceous gland proliferation and sebocyte lipogenesis. Many acne patients show heightened androgen sensitivity or increased local enzyme activity (e.g. 5α-reductase) in the sebaceous unit. (Medscape)
- IGF-1 / Insulin signalling: Elevated insulin and insulin-like growth factor 1 (IGF-1), often seen in high-glycemic diets, obesity, or insulin resistance, can stimulate sebaceous lipogenesis and reduce expression of FoxO transcription factors, which implicitly regulate proliferation and differentiation in sebocytes. (IJDVL)
- Sebocyte intrinsic dysregulation: Some sebocytes may have inherent predisposition to hyperlipogenesis or defective autophagy/mitophagy mechanisms. Research suggests oxidative stress, lipid peroxidation (especially of squalene), and mitochondrial dysfunction within sebocytes can exacerbate abnormal lipid production. (Frontiers)
- Hormonal fluctuations beyond androgens: Estrogen, progesterone, cortisol, and adrenal androgens (e.g. DHEA-S) can modulate sebum indirectly. For instance, cortisol (stress hormone) may upregulate sebogenesis via glucocorticoid receptors or via cross-talk on androgenic pathways. Some studies suggest that stress elevating cortisol may worsen acne. (PMC)
In Indian populations, data are sparser, but in dermatology journals of India, metabolic and endocrine investigations (e.g., in female acne / polycystic ovarian syndrome [PCOS]) often reveal subtle insulin resistance or hyperinsulinaemia even among “non-obese” acne patients. (However, these studies tend to focus on therapeutic interventions, less on quantifying sebaceous activity.)
Limitations / open questions:
- Why does acne often remit in the early twenties even though androgen levels remain? Some hypothesize that sebaceous gland responsiveness declines, or microbiome shifts happen, but the “remission paradox” remains partly unexplained. (JDDonline)
- Heterogeneity: Not all acne patients exhibit overt hyperseborrhea, indicating that sebum overproduction is necessary but not sufficient in genesis.
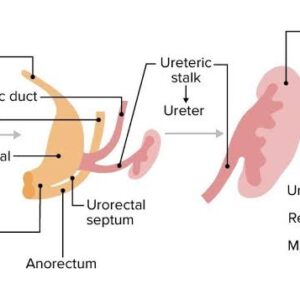
2. Follicular Hyperkeratinization and Ductal Plugging
Even if sebum is abundant, acne lesions cannot form unless the follicular duct (infundibulum) becomes obstructed. This arises from the abnormal shedding (desquamation) of keratinocytes and accumulation of corneocytes at the infundibular region, forming a microcomedone, the initial lesion (often subclinical).
Mechanistic details:
- Keratinocyte proliferation and cohesion changes: Upregulation of cytokeratins (e.g. K16, K17), altered desmosomal adhesion, and reduced shedding of cells can lead to plugging. (IJDVL)
- Role of IL-1, IL-1α, IGF-1: In uninvolved skin adjacent to acne lesions, IL-1 (a pro-inflammatory cytokine) may stimulate hyperproliferation of keratinocytes and abnormal cornification. (IJDVL)
- Influence of androgens and retinoid signaling: Androgens may indirectly influence follicular keratinization. Endogenous retinoid pathway defects (e.g. altered retinoic acid receptor expression) may predispose to abnormal desquamation.
- Barrier dysfunction / follicular epithelium changes: Some studies indicate that the infundibular epithelium in acne-prone skin has impaired barrier, altered lipid composition, or increased permeability to irritants. This facilitates deep penetration of proinflammatory molecules, lipids, and microbial metabolites.
- Oxidative stress & peroxidation: Lipid peroxidation products (e.g. oxidized squalene) may irritate the follicular epithelium, induce keratinocyte proliferation and desmoglein alteration, enhancing comedone formation.
Thus, microcomedones arise before clinically visible lesions; growth of sebum and bacterial proliferation then convert them to visible comedones, papules, pustules, or nodules. (NCBI)

3. Microbial Colonization and Dysbiosis
Once the follicular duct is plugged, the microenvironment becomes anaerobic and rich in lipids—favorable for colonization by Cutibacterium acnes (C. acnes, formerly Propionibacterium acnes). But the mere presence of C. acnes is not pathogenic; the key is strain diversity, dysbiosis, immune response, and virulence factors.
Salient features:
- Strain heterogeneity: Multiple phylotypes / strains of C. acnes exist (IA1, IB, II, III, etc.). Some are more inflammatory than others. Acne lesions more often harbor phylotype IA1, while healthy skin may have more IB or II, reflecting a shift in microbial community (dysbiosis). (Frontiers)
- Virulence factors: Lipases, proteases, porphyrins, CAMP factors, chemotactic factors, and biofilm formation may contribute to tissue injury, inflammation, and immune activation. For example, porphyrin production triggers reactive oxygen species (ROS). (Frontiers)
- Biofilm & colonization resilience: Some C. acnes strains form biofilm inside follicles, shielding themselves from immune attack or antimicrobials.
- Interactions with commensals: Dysbiosis may involve reduction in beneficial commensals (e.g. Staphylococcus epidermidis, Corynebacterium) or shifts in proportion; this is emerging as a concept via computational microbiome modeling. (arXiv)
- Immune activation: C. acnes triggers toll-like receptors (e.g. TLR2) on keratinocytes, sebocytes, and resident immune cells, promoting NF-κB activation and secretion of IL-1β, IL-6, IL-8, TNF-α, IL-17, and other inflammatory mediators. (IJDVL)
- Oxidative stress: ROS generation both by host inflammatory cells and by porphyrin oxidation contributes to lipid peroxidation, cell damage, and perpetuation of inflammation. (Frontiers)
From mathematical modeling perspectives, shifts in skin pH or environmental perturbations can push the microbial ecosystem from stable equilibrium into a dysbiotic, acne-prone state. (arXiv)
In Indian milieu: There is limited published genomic strain-specific data of C. acnes in Indian acne patients; future research is needed. However, Indian dermatology literature frequently acknowledges the microbial factor (though often generically) as critical, and some trials of topical antibiotics/benzoyl peroxide in Indian patients lend indirect support.
4. Inflammation and Immune Response
Where newer research has deepened understanding is in the central role of inflammation, now viewed not just as a downstream consequence of microbial invasion, but oftentimes as an early, initiating event, even before C. acnes overgrowth.
Highlights of the inflammatory mechanisms:
- “Silent inflammation” in clinically uninvolved skin: Studies show that in skin adjacent to acne lesions, there is baseline upregulation of IL-1, TNF-α, cathelicidin, toll-like receptors, and vascular adhesion molecules—even before visible disease. This suggests that inflammation is not purely secondary but part of the genesis. (IJDVL)
- Cytokine cascades: Activation of NF-κB in keratinocytes, sebocytes, and immune cells leads to expression of IL-1α, IL-8, IL-6, TNF-α, IL-17, IL-23, and IL-20, etc. These cytokines recruit neutrophils, monocytes/macrophages, Th17 cells, and mast cells, driving lesion formation. (IJDVL)
- Inflammasome activation: Some studies implicate the NLRP3 inflammasome in IL-1β activation within the follicle, contributing to comedone inflammation.
- Complement activation: C. acnes may trigger complement pathways (e.g. C3a, C5a) facilitating inflammation and leukocyte chemotaxis.
- Matrix metalloproteinases (MMPs) and tissue remodeling: MMPs (e.g. MMP-1, -9) released by keratinocytes and inflammatory cells degrade extracellular matrix, weakening follicular walls and facilitating rupture, leading to deeper inflammatory lesions and scarring. (IJDVL)
- Oxidative stress / ROS / lipid peroxidation: As noted, ROS amplify cytokine release, damage lipids and proteins, and perpetuate inflammation in a vicious cycle.
- Neurogenic inflammation: Emerging evidence suggests that neuropeptides (e.g. substance P, CGRP) released by cutaneous nerve endings under stress may modulate local inflammatory milieu and sebocyte responses.
- Innate-adaptive immune cross-talk: Dendritic cells, Langerhans cells, and T cells (especially Th17) may orchestrate sustained inflammation in persistent acne.
In Indian dermatological reviews, the importance of cytokine polymorphisms (e.g. TNF-α-308, IL-1β) has been explored as susceptibility factors in acne pathogenesis. (IJDVL)

5. Genetic and Epigenetic Predisposition
No discussion of acne etiology is complete without genetics. Familial clustering and twin studies strongly support heritability.
Key findings:
- Twin studies report heritability of acne traits as high as ~ 80% in some populations. (PMC)
- Epidemiological meta-analysis: family history is consistently a major risk factor for both development and severity of acne. (Nature)
- Polymorphisms in genes related to inflammation (TNF, IL-1, TLR2), androgen metabolism (e.g. CYP17, SRD5A2), and sebaceous differentiation have been studied. For example, TNF-α-308 polymorphism is a candidate in Indian dermatology literature. (IJDVL)
- Epigenetic regulation (DNA methylation, histone modifications, microRNAs) is an emerging field: some studies suggest that miRNAs regulating lipogenesis, inflammation, or keratinocyte differentiation may influence acne susceptibility (though far from clinical translation).
- Gene-environment interactions: A genetically susceptible individual may require triggers (diet, stress, microbiome shift) to manifest clinically.
In India, some research has attempted to correlate certain HLA types or cytokine gene polymorphisms with acne, but findings remain inconclusive and sample sizes small.
6. Metabolic, Dietary, and Hormonal Modulators
Beyond the classical factors, recent research has increasingly focused on diet, metabolic syndrome / insulin resistance, BMI, and related hormones as modulators.
Major points:
- High-glycemic load diets: Many studies correlate high glycemic index (GI) or glycemic load (GL) diets with increased acne severity. High GI foods raise insulin and IGF-1, which in turn stimulate sebogenesis, reduce sex hormone binding globulin (SHBG), and promote androgen activity. (PMC)
- Dairy consumption: Some meta-analyses show modest associations between milk (especially skim milk) and acne, possibly mediated via insulinotropic hormones in milk (IGF-1, insulin). However, causality remains debated. (PMC)
- Obesity and adipokines: Obesity is associated with increased insulin resistance and elevated leptin, adiponectin dysregulation, and altered inflammatory milieu. The linkage between obesity and acne is not straightforward, but some studies (especially in China) show correlation. (PMC)
- Metabolic syndrome components: Elevated triglycerides, LDL, and lower HDL have been observed in subsets of acne patients, possibly aggravating oxidative stress and inflammation.
- Hormonal disorders (e.g. PCOS): In females, PCOS is a classic model wherein androgen excess, insulin resistance, and altered SHBG contribute to persistent or late-onset acne. Many dermatology and endocrinology studies in India examine PCOS-associated acne and its severity.
- Stress hormones and HPA axis: Chronic psychological stress activates the hypothalamic-pituitary-adrenal (HPA) axis, raising CRH, ACTH, and cortisol, which may upregulate sebaceous lipogenesis and potentiate inflammation. CRH receptors are expressed in sebaceous glands and keratinocytes.
- Menstrual cycle fluctuation and acne flares: Recent studies (e.g. Jain et al, 2025) confirm periodic flares in acne tied to luteal-phase hormonal changes (elevated progesterone, androgen fluctuations) in many women. (ScienceDirect)
Thus, metabolic and hormonal modulators act as amplifiers of the core pathophysiologic mechanisms.
7. Environmental and Lifestyle Contributors
These are often overlooked but can tip the balance toward expression of acne in predisposed individuals.
- Dietary supplements / medications: Drugs with androgenic effects (e.g. testosterone, anabolic steroids, lithium, corticosteroids) can provoke acneiform eruptions. (Wikipedia)
- Cosmetics / comedogenic topical agents: Use of heavy oils, petrolatum, comedogenic makeup or hair oils (pomade acne) can plug follicles and worsen acne, especially in darker skin types. (DermNet®)
- Humidity, sweating, friction (occlusion): In tropical or humid climates (such as many parts of India), sweating and occlusive clothing can exacerbate follicular plugging and microbial growth.
- Ultraviolet (UV) radiation / photodamage: UV may worsen oxidative stress, lipid peroxidation, and barrier damage. Some acne-adjacent research suggests UV-induced free radicals can aggravate lesions.
- Smoking: The link with acne vulgaris is controversial, but smoking has been associated with a subtype of non-inflammatory “smoker’s acne” (APAA). Free radicals from smoke might peroxidize lipids in sebum. (Verywell Health)
- Pollution / air particulate matter: Environmental pollutants may oxidize skin lipids, damage barrier, and induce low-grade inflammation; though robust direct human data are limited.
- Sleep deprivation / circadian disruption: Poor sleep, shift work, or circadian misalignment may dysregulate hormonal and inflammatory pathways, indirectly exacerbating acne.
- Psychosocial stress: As a precipitant or exacerbator, stress is important (discussed further below).
- Hygiene / skin cleaning: Over-washing or harsh cleansers can disrupt barrier function, increase irritation, and sometimes paradoxically worsen acne; whereas under-washing alone is not a primary cause. (PMC)

Environmental/lifestyle factors are essentially modifiers—they rarely cause acne alone but shape its severity and persistence.
8. Psychological, Neuroendocrine and Psychosocial Interactions
One of the must-not-ignore dimensions is the mind–skin interaction in acne. Psychological stress and associated neuroendocrine changes not only influence disease severity but may contribute to onset in some individuals.
Mechanisms and evidence:
- HPA axis activation, CRH, and neuropeptides: Stress stimulates CRH (corticotropin-releasing hormone), which can act locally in skin to upregulate sebaceous lipogenesis, cytokine release, and vascular responses. Sebocytes express CRH receptors.
- Neuropeptides (e.g. substance P, vasoactive intestinal peptide, calcitonin gene–related peptide) may modulate keratinocyte and sebocyte behavior under stress, enhancing inflammation locally.
- Behavioral patterns: Stress may increase face-touching, picking, use of heavy cosmetics, or poor sleep, all of which exacerbate acne indirectly.
- Psychiatric comorbidity: Acne is well known to be associated with depression, anxiety, low self-esteem, body image disturbance, social withdrawal, and even suicidal ideation. (PMC)
- Example: A cross-sectional study among adolescents in Ahmedabad (India) showed severity of acne correlated significantly with lower self-esteem, social anxiety, and negative self-perception. (SeeJPH)
- A 2023 psychology study (Tasneem et al) reported that higher acne severity predicted higher anger, anxiety, and depression in youth populations. (Frontiers)
- A 2023 review of skin disease and psychosocial burden highlighted intricate feedback loops: acne exacerbates stress and negative emotions, which further worsen acne (a vicious cycle). (PMC)
- Sleep disturbance and depression: Poor sleep worsens both mood and systemic inflammation, which may influence acne.
- Adolescence as critical period: Because acne typically peaks in adolescence, the impact on identity, appearance, and social functioning is profound and may itself create stress that perpetuates disease.
- Quality-of-life studies in India: The Indian scenario, as in global studies, shows that acne patients frequently report embarrassment, social avoidance, and impaired quality of life, often seeking cosmetic dermatology treatments. (ResearchGate)
Therefore, psychological state is not an epiphenomenon but an important modulator of acne expression, persistence, and treatment response.
Integrative Etiologic Model (Synthesis)
From the above, we can visualize acne vulgaris as a multi-hit disease in which multiple parallel and sequential pathways interact:
- Genetic/epigenetic predisposition sets a baseline susceptibility (sensitivity of sebocytes, keratinocytes, immune thresholds).
- Hormonal / metabolic milieu (androgens, insulin/IGF-1, stress hormones) provides the drive for sebum overproduction and modulates keratinocyte behavior.
- Local changes in the follicular environment (lipid peroxidation, barrier dysfunction, microenvironment hypoxia) predispose to plugging and oxidative stress.
- Microbiome dysbiosis (overgrowth of inflammatory strains of C. acnes) triggers immune activation via TLRs, inflammasomes, complement, and chemokines.
- Inflammation, both innate and adaptive, propagates lesion development, follicular wall rupture, further immune recruitment, MMP-mediated tissue damage, and scarring.
- Modifying factors (diet, lifestyle, stress, environment, cosmetics) amplify or dampen these processes.
- Psychoneuroimmune feedback loops: Stress worsens hormonal and immune dysregulation, which worsens acne; the acne itself adds psychological burden, forming a vicious cycle.
In practice, different patients may have dominance of one or more pathways (sebogenic acne, inflammatory acne, diet-sensitive acne, stress-sensitive acne). This has implications for individualized therapy.
Research Updates and Gaps (Global and India-Relevance)
Here are some of the noteworthy recent developments and the lacunae:
- Novel anti-inflammatory targets: Research is exploring inhibitors of IL-17, IL-1, inflammasome modulators, JAK-STAT inhibitors, and microbiome-modulating agents (e.g. bacteriophage therapy). (Frontiers)
- Squalene oxidation inhibitors / antioxidants: Targeting lipid peroxidation with topical or systemic antioxidants (e.g. N-acetylcysteine, niacinamide, botanical antioxidants) is under investigation. (Frontiers)
- Probiotics / prebiotics / microbiome therapies: Modulating the skin or gut microbiome to favor protective strains is being studied. (Frontiers)
- Non-antibiotic antimicrobials / bacteriophage approaches: To avoid antibiotic resistance, non-antibiotic antibacterial agents and phage therapies are in exploratory stages. (Frontiers)
- Genomic & multi-omics studies: Integrated transcriptomic, proteomic, and metabolomic profiling of acne lesions is emerging, but with limited data in Indian populations.
- Indian-specific epidemiology and biochemical studies: The “Systematic Review of the epidemiology of acne vulgaris” (Nature, 2020) included Indian studies and found that family history, body mass index, and skin type are significant risk modifiers. (Nature)
- National guidelines and consensus: The recent PRACT-India (2025) provides practical recommendations for acne care tailored for Indian practice, acknowledging limitations and recommending psychological screening. (MDPI)
- Psychosocial research in India: While small cross-sectional studies exist (e.g. Ahmedabad, knowledge-attitude surveys), large longitudinal or interventional studies on how psychological therapy influences acne outcomes are lacking.
- Therapeutic trials in Indian populations: Many trials in Indian dermatology journals test topical agents, Ayurvedic combinations, or diet-based interventions, but rigorous mechanistic correlation (e.g., linking change in cytokines, sebum lipids, microbiome) is rare.
- Gaps:
• Lack of large-scale Indian multi-omics data.
• Sparse data on pediatric vs adult-onset acne distinctions in Indian cohorts.
• Few controlled trials that integrate psychological interventions with dermatologic care.
• Need for strain-level C. acnes mapping in Indian skin types.
• Need for longitudinal studies mapping diet, insulin resistance, and acne progression in Indian adolescents.
Thus, while the global literature is rich, for Indian practice there is room for deeper integrative studies combining Ayurvedic principle-driven biomarkers with molecular dermatology.
Comments / Perspective from Renowned Dermatologists
To give perspective, here are some viewpoints drawn from leading dermatologist authors:
- Many modern dermatologists emphasize that inflammation is not merely a late event, but may start early—even in subclinical microcomedones, so anti-inflammatory therapy early may forestall lesion formation.
- Some dermatology reviews caution that antibiotic monotherapy is outdated, because targeting upstream (sebum, keratinization, microbiome balance) is more sustainable.
- Others advocate individual phenotype-based therapy: a patient with high glycemic diet, insulin resistance, and sebum dominance might benefit from metabolic interventions; another with stress-exacerbated acne might benefit from psychodermatology support.
- In Indian dermatology commentary, many call for integration of lifestyle, diet, behavioral counseling alongside pharmacotherapy, especially given differences in skin types, climate, and patient expectations in India.
These perspectives resonate with an integrative approach—precision therapy targeting the dominant etiologic axis in each patient.
The Psychological and Chemical Interplay – More Depth
Because you as an Ayurvedic scholar may be particularly interested in mind-body dynamics, here is a deeper dive into how psychology, neurochemistry, and skin biochemistry intertwine in acne.
- Stress and Neuroimmune Signaling
- Psychological stress elevates CRH, ACTH, cortisol, neuropeptides (e.g. substance P), and sympathetic outflow.
- CRH is expressed in skin (keratinocytes, sebocytes) and can enhance sebaceous lipogenesis and pro-inflammatory cytokines.
- Substance P promotes vasodilation, mast cell degranulation, and cytokine release—all of which may worsen lesion inflammation. - Cytokine-Mood Interactions
- Systemic inflammation (e.g. IL-1, IL-6, TNF) can cross-talk to brain circuits, contributing to mood symptoms (sickness behavior, anhedonia).
- In acne, elevated cytokines may contribute to subclinical mood alterations, particularly in susceptible individuals. This may partly explain higher rates of depression in acne patients. - Oxidative Stress & Neurotransmitters
- Oxidative stress in skin can mirror systemic oxidative stress. Elevated ROS are also implicated in neuropsychiatric disorders.
- The glutathione system, NADPH oxidases, and antioxidant enzymes create a biochemical link between skin state and systemic redox balance. - Sleep, Melatonin, and Circadian Regulation
- Disrupted sleep alters melatonin, cortisol rhythms, and inflammatory cytokines, which may feed into acne exacerbation.
- Melatonin (a potent antioxidant) is also synthesized in the skin; altered melatonin signaling may influence local oxidative stress and barrier function. - Behavioral Feedbacks
- Anxiety or body-image distress may promote compulsive skin-picking (excoriation), overuse of topical agents, or adherence lapses, each aggravating lesions.
Clinically, this argues for holistic care: dermatologic treatment plus psychological support, stress management, sleep hygiene, and perhaps even mind-body therapies (yoga, meditation) which might modulate systemic inflammation and neuroendocrine balance.

Treatment Implications (Therapeutic Principles)
Given the etiologic depth, the therapeutic strategy should not merely suppress lesions, but rebalance the pathophysiologic network. Some guiding principles (without going into full protocols):
- Early incorporation of anti-inflammatory agents (e.g. topical retinoids, non-antibiotic anti-inflammatories) to suppress subclinical inflammation.
- Use of comedolytic agents (retinoids) to normalize keratinocyte shedding and prevent ductal plugging.
- Careful modulation of sebaceous lipogenesis, including hormonal therapy (oral contraceptives, spironolactone in females), insulin-sensitizing therapy (metformin in PCOS-associated acne), and antioxidants / lipogenesis inhibitors.
- Judicious use of antimicrobials, ideally in combination (e.g. benzoyl peroxide, topical antibiotics, systemic antibiotics), but always with resistance prevention in mind.
- Adjunctive antioxidants, photoprotection, and barrier-restorative agents.
- Lifestyle and dietary counseling (low GI diet, reduce dairy, weight control, sleep hygiene).
- Psychological support: screening for depression/anxiety, cognitive-behavioral therapy, stress management.
- Emerging therapies targeting microbiome modulation, cytokine inhibitors, and non-antibiotic antimicrobials will likely refine personalized regimens.

From the Ayurvedic perspective, one could imagine combining gentle internal purification (e.g. blood/pitta balancing), topical herbal formulations that modulate sebum and inflammation, along with mental-emotional balance as adjuncts—so long as they are grounded in contemporary mechanistic insight.
Conclusion & Suggestions for Future Research
Acne vulgaris must be conceptualized as a multi-layered, systemic disorder manifesting in the skin’s pilosebaceous units. The classical four-pathway model (sebum, keratinization, microbes, inflammation) remains foundational, but must be expanded to include genetics, metabolic modulation, neuroimmunology, psychological stress, and environmental modifiers.
For your practice as an Ayurvedic scholar, the strengths lie in an integrative lens—identifying which etiologic axes (e.g. metabolic, stress, dietary) dominate in a given patient and tailoring holistic support in tandem with rational modern therapy.
Key research frontiers you might consider in your own setting (or in collaboration) include:
- Conducting phenotype-based observational studies in your patient population (e.g. linking metabolic markers, Ayurvedic prakriti, psychological metrics, and inflammatory biomarkers).
- Undertaking interventional trials where Ayurvedic regimen (diet, rasayana, panchakarma) is adjuncted to modern therapy, with readouts including cytokines, sebum lipid profiles, microbiome shifts.
- Investigating the skin and gut microbiome in Indian acne patients, especially strain-level C. acnes mapping.
- Longitudinal studies of psychological interventions (mindfulness, yoga) as acne adjuncts, measuring both clinical and biochemical endpoints.
By approaching acne as a systems disorder (not just a skin lesion), you position your practice as ahead of many purely symptomatic dermatology models.
References
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. American Academy of Dermatology. Journal of the American Academy of Dermatology. 2016;74(5):945–973. https://doi.org/10.1016/j.jaad.2015.12.037
- Thiboutot D, Gollnick H, Bettoli V, et al. New insights into the management of acne: An update from the Global Alliance to Improve Outcomes in Acne Group. Journal of the American Academy of Dermatology. 2009;60(5 Suppl):S1–S50.
- Bhate K, Williams HC. Epidemiology of acne vulgaris. British Journal of Dermatology. 2013;168(3):474–485. https://doi.org/10.1111/bjd.12149
- Zouboulis CC, Jourdan E, Picardo M. Acne is an inflammatory disease and alterations of sebum composition initiate acne lesions. Journal of the European Academy of Dermatology and Venereology. 2014;28(5):527–532.
- Dessinioti C, Katsambas A. The role of Propionibacterium acnes in acne pathogenesis: facts and controversies. Clinical Dermatology. 2010;28(1):2–7.
- Dreno B, et al. Microbiome in acne vulgaris: a review. Journal of the European Academy of Dermatology and Venereology. 2018;32(12):2105–2114.
- Ghosh S, Chaudhuri S. A clinical study on the management of acne vulgaris with Ayurvedic formulations. AYU (An International Quarterly Journal of Research in Ayurveda). 2012;33(4):543–546.
- Nandini D, Raveendra L, et al. Prevalence and risk factors of acne vulgaris among adolescents in India. Indian Journal of Dermatology, Venereology and Leprology. 2014;80(3):283–289.
- Khunger N, Kumar C. Psychosocial effects of acne vulgaris: A study among adolescents in India. Indian Journal of Dermatology. 2012;57(1):26–29.
- Sharma PV. Charaka Samhita (Text with English Translation). Chaukhamba Orientalia, Varanasi.
- Murthy K.R.S. Sushruta Samhita (English Translation). Chaukhamba Publications.
- Tripathi B. Ashtanga Hridaya with English Commentary. Chaukhamba Sanskrit Pratishthan.
- Dawson AL, Dellavalle RP. Acne vulgaris. BMJ. 2013;346:f2634. https://doi.org/10.1136/bmj.f2634
- Tan JK, Bhate K. A global perspective on the epidemiology of acne. British Journal of Dermatology. 2015;172(Suppl 1):3–12.
- Williams HC, Dellavalle RP, Garner S. Acne vulgaris. The Lancet. 2012;379(9813):361–372.
Our Other articles
Food Safety and Standards Act, 2006: Ensuring Safe & Healthy Food for India
Psoriasis: Modern and Ayurvedic Perspectives
Disclaimer: This article is based on multiple credible sources and expert opinions. AI tools were used to compile and structure the content. It is not a substitute for professional medical advice.






Pingback: Acne Vulgaris: Integrative Ayurvedic and Modern Therapeutic Protocols -
Pingback: Acne Vulgaris: Diagnostic Aspects and Clinical Assessment – An Integrative Ayurvedic and Modern Perspective -